Abstract
Background:
Patients with sickle cell disease (SCD) are at increased risk of developing serious infections as a result of functional asplenia and altered humoral immunity. Nevertheless, presenting symptoms of sepsis such as fever and arthralgias are common in SCD and can occur with many sickle cell related conditions, including vaso-occlussive crises (VOC) and may not correlate with true infections. The neutrophil-to-lymphocyte ratio (NLR) is calculated as the absolute neutrophil count divided by the absolute lymphocyte count and represents an easily accessible value that has been found to correlate with inflammation and prognosis in several conditions. Few studies have evaluated NLR as a biomarker in sickle cell disease, and its utility in differentiating infection vs. VOC in patients presenting to the emergency room remains unknown.
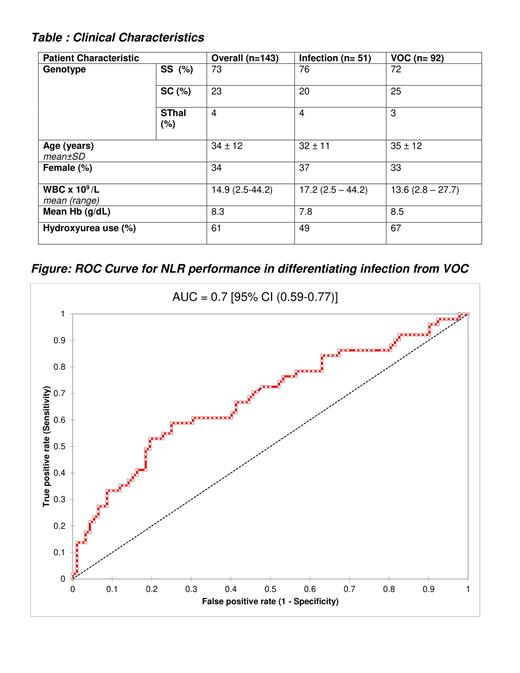
Method: We conducted a retrospective review of 143 patients with SCD who presented to the emergency department with fever and painful crises. The patients were divided into two categories based on discharge diagnoses - patients with VOC only (n=92) and patients with proven/possible infection (n=51). Inclusion criteria for both groups were patients with SCD, 17 years and older and complete blood count with differential on presentation; patients who had received antibiotics prior to presentation were excluded. Data collected on presentation included genotype, age, gender, complete blood count, hydroxyurea use. Data was analyzed between the two groups using descriptive statistics and receiver-operating characteristic (ROC) curve analysis.
Results: Demographics and clinical characteristics are summarized in the Table. The sample included primarily young adult males with 61% on hydroxyurea. Genotype HbSS (73%) was most prevalent followed by HbSC (23%) and HbSβ (4%). The mean Hb was around 8 g/dL. The VOC group had a lower mean white blood cell (WBC) count of 13.6, compare to 17.2 for patients with proven/possible infection. ROC analysis showed that NLR did correlate with infection, with a modest AUC 0.7 [95% CI (0.59-0.77)] that was significant (p=0.0002) when compared to the AUC=0.5 model. Maximum specificity and sensitivity in this sample was achieved with NLR = 4.5 (Specificity 75% and Sensitivity 59%).
Conclusion: In this sample, NLR on presentation significantly but only modestly correlated with infection as opposed to VOC. Optimal performance at NLR=4.5 achieved Specificity 75% and Sensitivity 59%. Despite modest performance, given the widespread availability and cost-effectiveness of NLR testing, further study in a larger sample may derive other variables that can combine with NLR to formulate a predictive model to improve care for these patients.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal